The healthcare industry is undergoing a digital revolution, with artificial intelligence and automation technologies transforming how medical organizations manage administrative tasks. The industry’s most challenging issues, including patient care workflow streamlining and regulatory compliance, are being addressed through such innovation.
One of the most significant improvements is currently underway in the area of prior authorization and grievance management, with offerings becoming more innovative, quicker, and more patient-centric.
Key Takeaways
- AI in healthcare is revolutionizing the administration of medical organizations by addressing burdens like prior authorization and grievance management.
- Automation technologies help reduce wait times and improve patient access by streamlining workflows and enhancing efficiency.
- Innovative grievance management systems use natural language processing to prioritize complaints and improve patient satisfaction while ensuring regulatory compliance.
- Interoperability is crucial, allowing various healthcare systems to integrate and share data seamlessly, which facilitates better patient care.
- The future involves leveraging AI and automation to enhance operational efficiency, predict patient needs, and improve the overall healthcare experience.
Table of Contents
- The Growing Burden of Healthcare Administration
- AI-Powered Prior Authorization: Reducing Wait Times and Improving Patient Access
- Innovative Grievance Management: Enhancing Patient Satisfaction and Regulatory Compliance
- Interoperability and Integration: The Foundation of Effective Healthcare Technology
- The Impact on Patient Care and Healthcare Economics
- Looking Toward the Future
The Growing Burden of Healthcare Administration
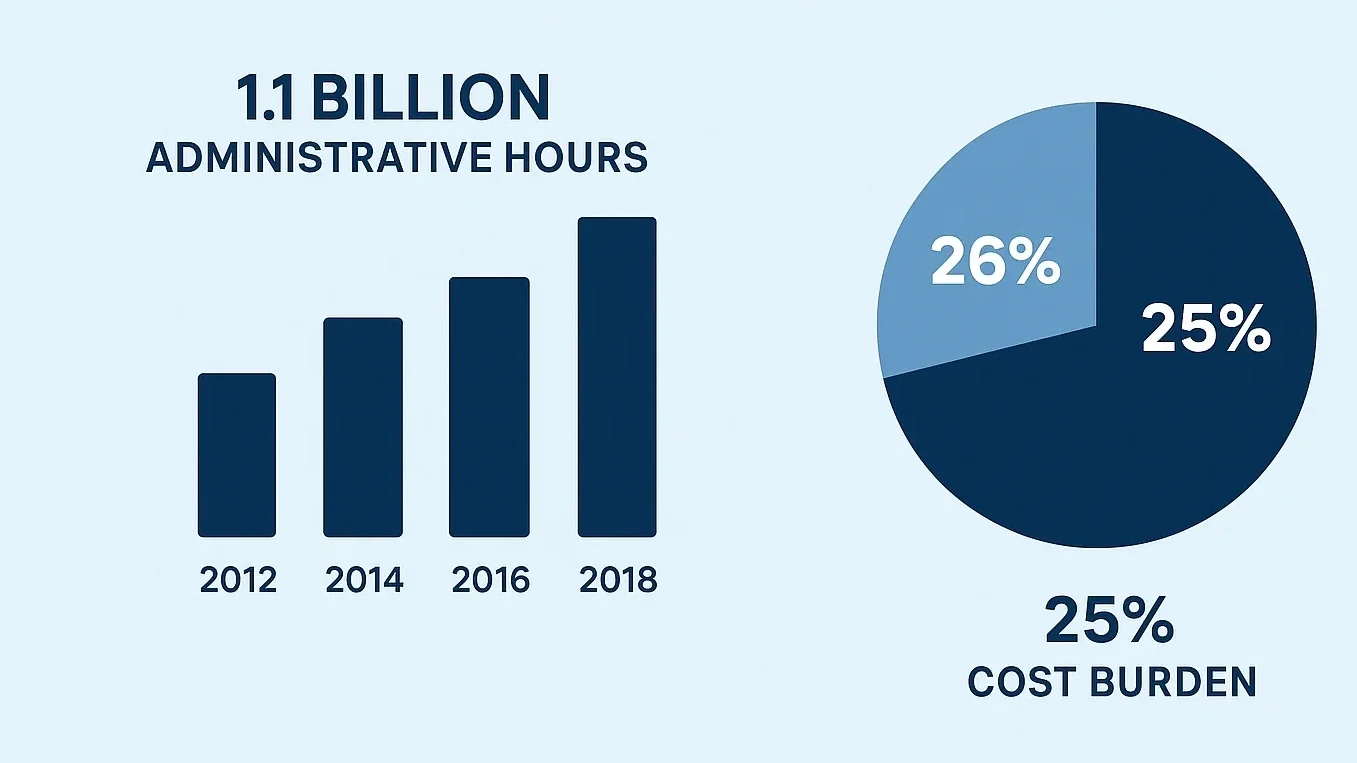
The Increased Administrative Load on Healthcare Providers. Providers are currently under pressure to increase the speed of administrative task completion with minimal errors and continue to meet regulatory compliance. For example, prior authorization alone has a direct impact on millions of patients each year. However, most current processes are managed manually, which often leads to unnecessary time delays and ultimately poorer patient outcomes. Recent studies have reported that healthcare companies spend billions of hours each year on administrative tasks that can be optimized through the adoption of intelligent automation. Market-leading healthcare technology firms are responding to these challenges with new offerings, with some focusing particularly on the complex workflows and subtasks within prior authorization and grievance management.
The rules and regulations surrounding many aspects of the healthcare industry have become increasingly complex, particularly guidelines from the Centers for Medicare & Medicaid Services (CMS), which impose significant demands on organizations to maintain accurate records and meet specific deadlines. The time and money required to meet administrative demands often come at the expense of other patient-facing tasks; however, this inefficiency can be resolved with innovative technology solutions.
AI-Powered Prior Authorization: Reducing Wait Times and Improving Patient Access
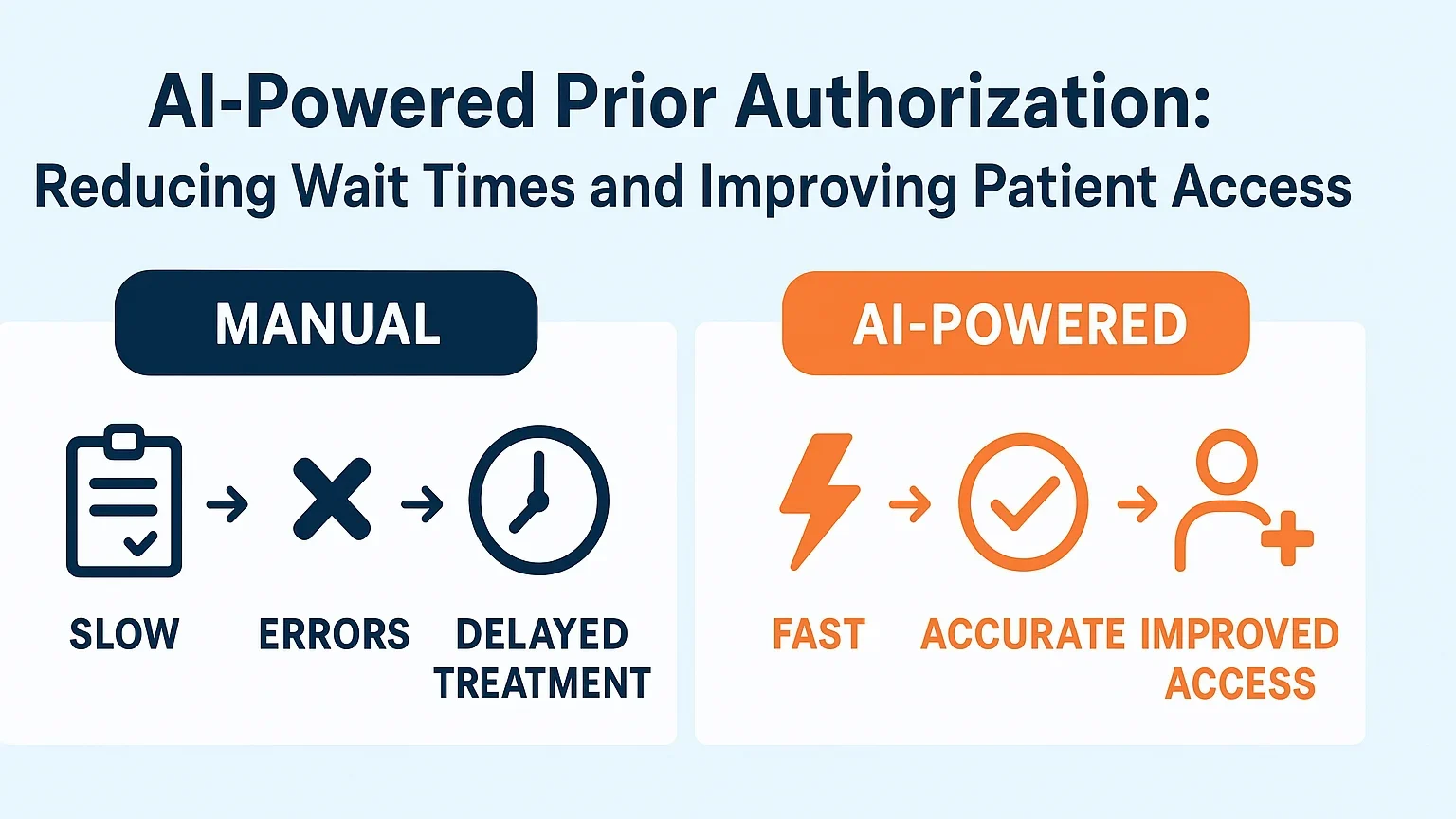
Smarter, Faster Prior Authorization with AI Assist. Current ePA solutions are utilizing artificial intelligence to shorten wait times and improve accuracy. For example, platforms that provide this functionality can scan medical records and compare treatment guidelines and coverage rules to automatically approve routine requests that fall within set parameters. Machine learning algorithms can improve over time. They identify patterns of approval and denial outcomes for both clinical and back-office analysis. They allow for the identification of common bottlenecks and suggest optimization points for the workflow.
Machine learning algorithms are continually enhanced by analyzing patterns in approval and denial decisions, helping businesses identify common bottlenecks. This technology is particularly valuable for specialty medications and procedures. Traditional prior authorization processes can create significant delays for patients requiring time-sensitive treatments.
The integration of real-time record exchange between healthcare vendors, pharmacies, and insurance companies further enhances efficiency. When a medical doctor prescribes a medication that requires prior authorization, computerized systems can immediately verify formulary requirements, patient eligibility, and medical necessity criteria, often providing immediate approval for straightforward cases.
Recent trends in electronic previous authorization platforms show this evolution in action. Advanced ePA portals now serve unique pharmacies, hub carrier agencies, and drug manufacturers, developing comprehensive ecosystems that expedite patients’ access to essential medicines. Much like a sequence analysis platform streamlines DNA and RNA workflows, these ePA systems integrate seamlessly with existing healthcare infrastructure while providing the necessary power for complex and distinctive drug authorization processes.
Advanced solutions, such as Agadia’s PAHub, demonstrate this evolution by providing unified systems that streamline the process of obtaining prior authorizations for both medical and pharmacy gains through a single interface. This interface also offers customizable workflows and real-time clinical decision support, which are essential for health plans to manage a wide range of medications, from routine to complex specialty drugs like GLP-1 therapies.
Innovative Grievance Management: Enhancing Patient Satisfaction and Regulatory Compliance
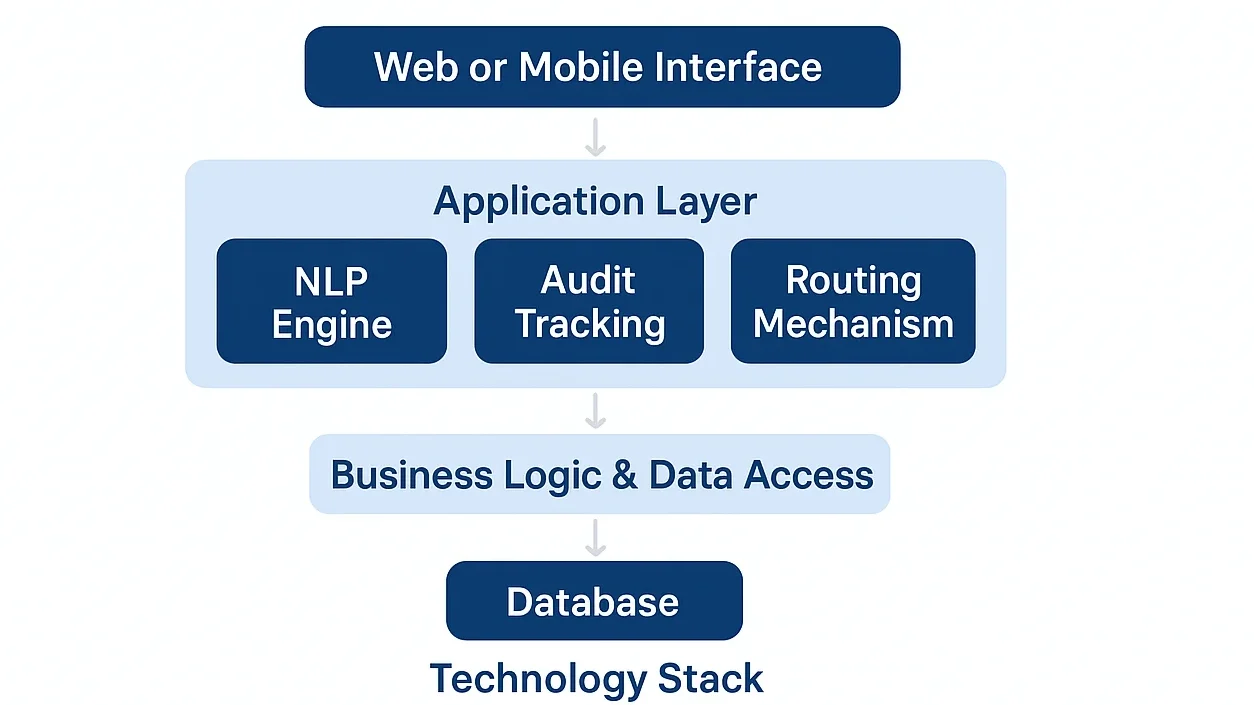
Grievance management systems have evolved from simple complaint-tracking tools into sophisticated platforms that ensure regulatory compliance while enhancing patient satisfaction. Modern solutions utilize natural language processing to categorize and prioritize complaints, automatically routing them accordingly.
This system’s tracking enables healthcare providers to gain insights into persistent complaints and trends in grievances. Allowing them to take action before problems worsen by maintaining comprehensive audit trails and utilizing automated reporting capabilities. Organizations can demonstrate regulatory compliance while allocating their human resources to complex cases that require personalized attention.
Advanced analytics enable healthcare administrators to understand the root causes of patient grievances, facilitating targeted improvements in service delivery. This data-driven approach transforms grievance management from a reactive process into a proactive tool for quality improvement.
Interoperability and Integration: The Foundation of Effective Healthcare Technology
The automation of the contemporary healthcare industry relies significantly on the seamless collaboration of stakeholders and various systems. The best possible answers will require the integration of electronic health records (EHR), pharmacy management systems, regulatory reporting systems, and other systems where seamless interfaces are needed.
Cloud-based architectures enable real-time data sharing while maintaining security and compliance with healthcare privacy regulations. This connectivity allows for more comprehensive patient care coordination and reduces the administrative burden on healthcare providers who previously had to navigate multiple disconnected systems.
API-driven integration capabilities ensure that automation tools can adapt to the diverse technology ecosystems found in healthcare organizations, from large health systems to specialty pharmacies and pharmaceutical manufacturers.
The Impact on Patient Care and Healthcare Economics
The transformation of healthcare administration through AI and automation extends far beyond operational efficiency. Patients experience faster access to needed treatments, reduced paperwork burdens, and more transparent communication about their care authorization status.
Staff engagement improves due to lower administrative costs, which drives their productivity in customer-facing tasks. The economic impact is substantial, with studies suggesting that widespread adoption of intelligent automation could save the healthcare industry billions of dollars annually while improving patient outcomes.
The newly established CMS rules support advances in electronic prior authorizations and reporting systems. They also explain the technology that health plans have to implement, and it is still a work in progress for many, particularly with the new CMS Interoperability and Prior Authorization Final Rule. This is an example of normative support, which motivates health organizations to further automate their administrative tasks.
Partnerships with technology providers become necessary for healthcare organizations. Agadia’s recent analysis of CMS compliance requirements highlights the specific technical and operational changes needed to meet these new standards.
Looking Toward the Future
The proliferation of healthcare technology will result in a more refined use of AI and automation in backend processes. AI will help organizations to predict and manage patient needs. With advanced conversational interfaces, providers, patients, and administrators will be able to communicate more easily and naturally.
The integration of blockchain technology will enhance the security and audit functionalities for sensitive patient health information. IoT devices can provide real-time monitoring data on patients for decision-making systems that enable automated treatment.
Organizations looking to implement these advanced healthcare automation solutions should partner with experienced technology providers. Who understand the complex regulatory landscape and can deliver comprehensive, compliant systems. Healthcare technology specialists like Agadia offer deep expertise in developing and implementing sophisticated prior authorization and grievance management platforms. Their recent insights on regulatory readiness and case work automation demonstrate how proper implementation of these systems strengthens both operational efficiency and regulatory compliance.
The future of healthcare administration lies in intelligent automation that enhances rather than replaces human expertise. By embracing these technological advances, healthcare organizations can create more efficient.