Each year, millions of people are threatened with permanent vision loss from eye diseases, and the risk is exceptionally high for someone with diabetes. But with the development of artificial intelligence (AI), retinal screening is becoming faster, more accessible, and more precise. AI-based retinal screening is already proving to do this in practice, helping prevent blindness and preserving vision for many.
Diabetic retinopathy (DR) affects approximately 35% of people living with diabetes worldwide, and nearly 10% of those affected experience some degree of vision loss. It is one of the leading causes of vision impairment globally and remains the primary cause of preventable blindness among working-age adults. Because DR often progresses without noticeable symptoms in its early stages, many patients are diagnosed only after irreversible damage has occurred, underscoring the critical need for timely and effective retinal screening.
Key Takeaways
- AI-powered retinal screening is transforming how we detect eye diseases, especially diabetic retinopathy.
- Diabetic retinopathy affects millions and can lead to irreversible vision loss without timely screening.
- AI screening offers scalability, cost-effectiveness, and improved access, particularly in underserved areas.
- While AI systems are effective, challenges like false positives and integration remain.
- Future advancements include hand-held devices and tele-ophthalmology, enhancing earlier detection and patient outreach.
Table of Contents
Why Retinal Screening Matters
Eye diseases such as Diabetic Retinopathy (DR) remain among the leading causes of vision loss worldwide. In the United States alone, out of an estimated 38.4 million people living with diabetes, approximately 26.4% have some form of diabetic retinopathy, and about 5.1% develop vision-threatening diabetic retinopathy (vtDR), the stage most likely to result in permanent vision loss. Despite these numbers, many cases still go undetected until the disease has progressed to a point where damage is difficult or impossible to reverse.
Conventional screening is based on manual analysis by ophthalmologists or trained graders of retinal fundus images. Although such an approach is extremely clinically effective, it is slow, dependent on resources and challenging to scale in rural or low-resource environments. Late presentations, insufficient referrals and specialist services shortages remain important contributors to avoidable blindness.
This is where AI starts to alter the equation. AI-enabled retinal screening systems present a high-throughput, scalable, and more accessible alternative to the traditional approaches, evidenced by growing evidence that has potential for early detection and reach at scale without accelerating existing eye-care resources.
What AI Retinal Screening Does and How It Works
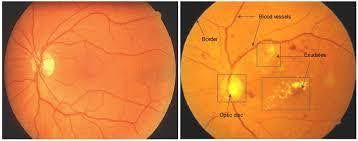
The positive screening 1 – x safety net. The AI retinal screening systems are based on deep learning models, which in turn are trained on large datasets of retinal images. These models are trained to detect early DR or other retinal diseases, such as microaneurysms, hemorrhages, exudates, and vascular changes. They can review new images rapidly (typically in under a minute) and identify cases that need more specialised attention.
A 2025 meta-analysis synthesizing dozens of studies reported that AI-based screening achieves a pooled sensitivity of ~90.5% (95% CI ~90.4–90.7%) and a specificity of ~78.3% (95% CI ~78.2–78.4%) for detecting diabetic retinopathy using fundus photographs.
For patients, that translates into early detection, frequently even before symptoms materialize. For health systems, it translates into scalable screening at a lower cost per screening and the possibility of lightening the load on ophthalmologists.
Evidence That AI Screening Works
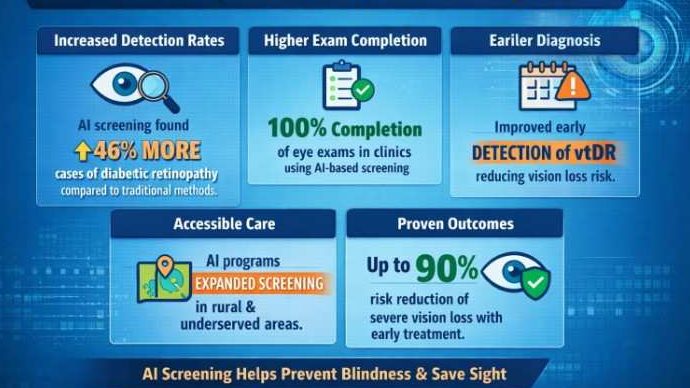
One notable long-term outcome study to consider is the CAREVL study. Investigators matched the results of autonomous AI screening with data from traditional eye‑care‑provider (ECP) exams during a 5-year period. Their model suggested that AI screening could prevent more vision loss than routine screening. In particular, they estimated that 27,000 fewer Americans would experience vision loss at 5 years with the AI strategy as compared with standard care.
“These findings underscore the actual preventive potential of early diagnosis combined with a screening test that is easy to get. The quicker turnaround time, high sensitivity and greater reach can make a substantial difference.
This potential is now being supported by recent clinical validation studies, helping address challenges similar to a monitor shadow issue that can obscure critical visual details. One such AI deployed in an ophthalmology clinic referred 100% of the cases of severe non-proliferative as well as proliferative DR, not missing any high-risk patient, as reported in a study in JAMA Network Open published in 2025.
EyeArt and Retmarker processed over 100,000 fundus images as part of the UK’s national diabetic eye‑screening program. They showed adequate sensitivity to detect referable DR, making them safe first‑level screening instruments compared with human graders.
These initiatives are proof AI doesn’t just keep up with human screening; in many cases, it means wider, quicker and earlier detection of eye disease where human resources are scarce.
Why AI Screening Outpaces Traditional Methods
Scalability
AI processes large numbers of retinal images rapidly. According to one platform evaluation, specific AI algorithms identified moderate‑to‑severe eye disease with 96.7–99.8% accuracy in under one second, a fraction of the time required for manual grading.
Access for Underserved Areas
Regions lacking retina specialists, rural zones, developing countries, and remote communities can now use fundus cameras and AI to screen large populations. This democratizes access to eye care and helps catch conditions early, even where care infrastructure is minimal.
Cost‑Effectiveness & Efficiency
AI reduces the per-patient cost of screening, decreases the need for repeated specialist visits, and minimizes specialist overwork. That makes routine screening sustainable at the national or public health scale.
Standardization & Objectivity
Unlike human graders who may vary in interpretation, AI applies the same criteria consistently across images, reducing variability, bias, and human error.
Challenges, Limitations & What Still Needs Work
AI screening isn’t flawless. Several challenges remain:
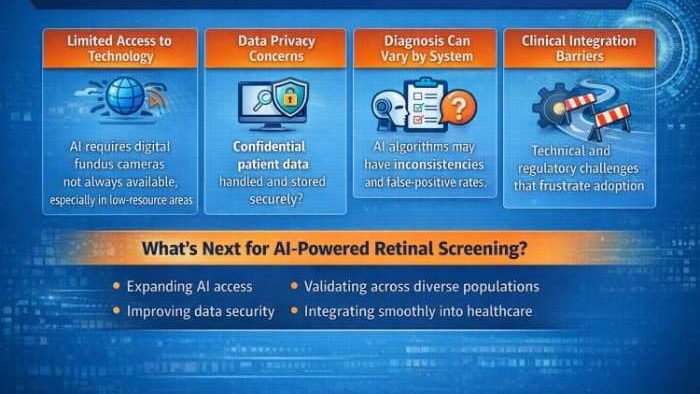
- False positives / low specificity: In some real‑world deployments, AI screening shows high sensitivity but modest specificity, leading to many false referrals and burdening specialists.
- Image quality and gradability issues: Cataracts, poor pupil dilation, or low‑resolution images can complicate AI performance. Some validated algorithms struggle in such scenarios.
- Follow-up adherence: Screening only matters if patients follow up. AI screening improves detection, but if patients don’t act on referrals, vision-loss prevention won’t happen. Models like CAREVL deliver the most significant benefit when patients adhere to recommended care.
- Regulatory and ethical concerns: Data privacy, algorithmic bias, and equitable performance across populations require careful governance.
- Integration challenges: Implementing AI screening requires compatible equipment (fundus cameras), trained staff, workflow changes, and robust data handling, all of which are not trivial in under-resourced settings.
What’s Next: The Future of AI in Eye Care
Several key paths are likely to see major change over the next few years:
- Hand-held screeners: New AI‑enabled hand-held fundus cameras recently cleared by the FDA have been touted as capable of having our screening process completely automated within a minute , and frequently even in primary-care or community settings.
- Tele‑ophthalmology + AI: Retinal images can be uploaded to cloud-based AI systems in remote clinics; patients in rural locations benefit from not having to travel far.
- Early detection beyond DR: Researchers are investigating the potential of AI-based detection of glaucoma, age-related macular degeneration, hypertensive retinopathy, and other eye diseases that fall beyond the reach of current retinal screening.
- Integrating into preventive care: A confluence of these and other AI-based screenings , along with diabetes care workflows, patient education, and real-time alerts, can significantly reduce the risk of vision loss.
AI‑powered retinal screening has the potential to become a standard preventive care tool worldwide, provided the necessary infrastructure and adoption are in place.
Health‑tech companies, hospitals, and public health agencies exploring such solutions will rely on robust AI pipelines and often partner with firms offering AI development services to build, validate, and deploy these screening platforms at scale.
Summary
AI‑powered retinal screening represents one of the clearest success stories in medical AI so far. It turns the possibility of early, scalable, accurate eye‑disease detection into reality, especially for populations that have lacked access to regular ophthalmic care.The technology isn’t perfect: false positives, image quality issues, adherence challenges, and system integration remain obstacles. But the data shows that, when implemented responsibly in collaboration with expert AI developers, AI screening can detect disease early, reduce the burden on specialists, and help prevent blindness for thousands.
Given the growing prevalence of diabetes worldwide and the ageing global population, expanding access to AI-powered retinal screening is no longer optional. It is necessary.










